Why is Good Data So Hard to Find?
Fast Healthcare Interoperability Resources (FHIR) was designed to unify data exchange to help address interoperability challenges in healthcare. However, real-world implementation has exposed a paradox: many EHR vendors rightfully claim compliance, yet their data remains incompatible. FHIR’s modularity and flexibility allow for adaptation, but this same flexibility leads to fragmented standards in practice, forcing clinics to handle unique “FHIR flavors” not always interoperable across systems (source).
Key Problems:
Multiple standards overlap, but do not converge automatically.
Each EHR product implements FHIR differently.
Data mapping often requires custom transformation for each hospital or clinic.
The result is a landscape where AI and analytics, modeled on clean FHIR standards, frequently run into real-world inconsistencies and data mismatches.
The Brittle Edge of Standardization
AI models required clean, well-structured data. In practice, clinical environments deliver inconsistent formats. These differences vary from semantic differences to diverse documentation habits. Even “standardized” FHIR data may suffer from missing fields or unique local modifications, undermining data-driven automation and predictive algorithms (source).
Why it matters:
AI systems trained on ideal data break down in local environments.
Variation leads to silent failures and hard-to-detect model errors.
A Text-Based and Flexible Future for Interoperability
Recent 2024 research highlighted a very creative alternative, combining FHIR modeling with natural language processing (NLP). Unstructured clinical notes and diagnostic reports, when interpreted by advanced AI, can be converted into structured FHIR-compatible formats while retaining rich nuance and accuracy.
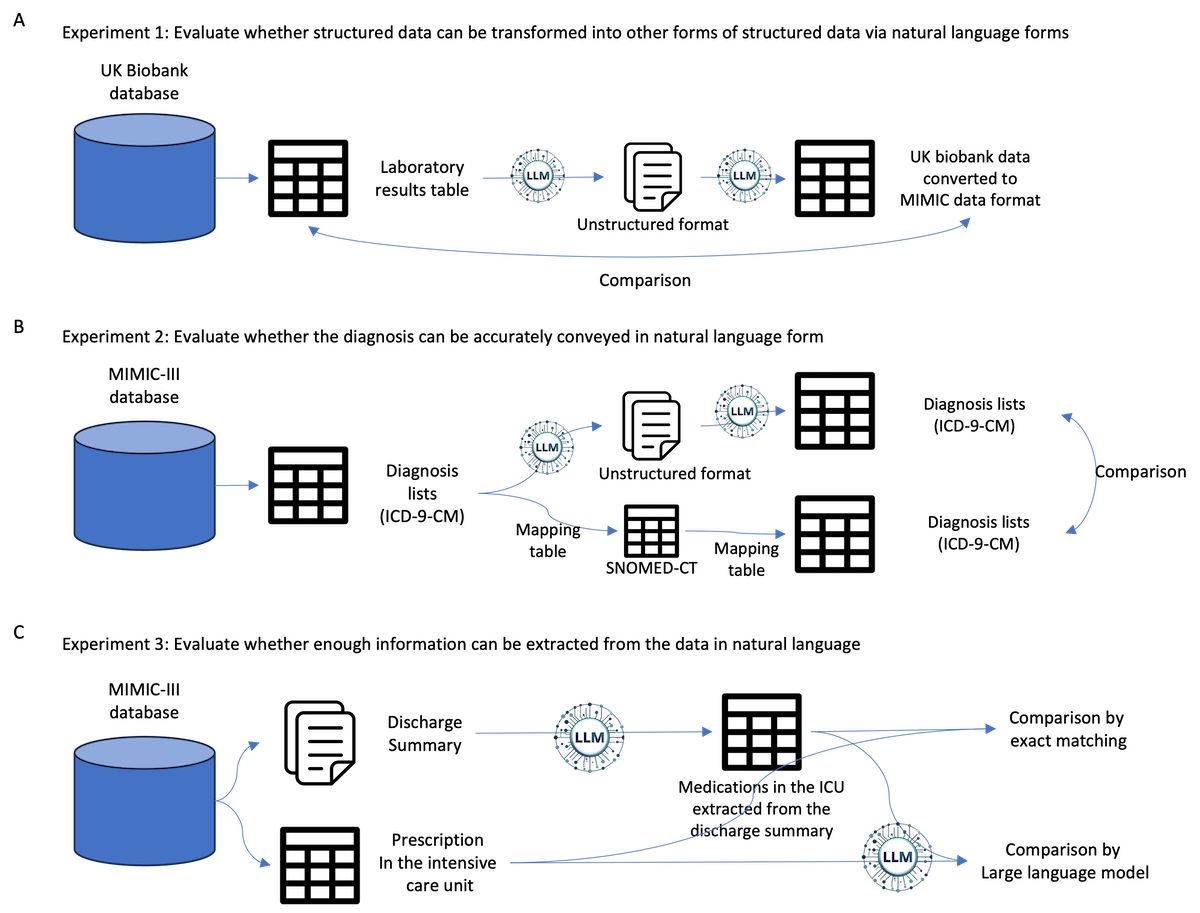
The research concluded that:
NLP techniques outperform rigid mapping for medication and diagnosis extraction.
Semantic preservation enables better patient context, especially for rare conditions.
Is this the future? Possibly, but not without overcoming significant hurdles. Challenges such as data privacy and compliance, model hallucinations, and the infrastructure costs make this approach difficult to adopt in the current healthcare ecosystem.
What Healthcare Teams Need to Know
To thrive in this evolving landscape, organizations should focus on these strategies:
Invest in modular platforms that can interpret both structured FHIR records and unstructured text.
Adopt tools that validate consistency and highlight missing or incompatible data.
Reduce manual mapping by leveraging smarter automation backed by clinical validation.
